When a patient is diagnosed with diabetes, it is a pivotal moment that demands a delicate and informative approach. This responsibility often falls on pharmacists, who play a crucial role in guiding patients through this new phase of their health journey. In this article, we will explore a structured method to assist pharmacists in effectively supporting patients with a recent diabetes diagnosis when they come to the pharmacy with a new prescription.
Initiating the conversation with the patient is key, and it goes beyond a mere exchange of information. Pharmacists should introduce themselves and confirm the patient's identity with a warm greeting. For example, "Hello, I'm Brian, the pharmacist here to assist you. Today, I'll be guiding you through some essential information about managing diabetes." Additionally, if a diabetes educator is available, their expertise can enhance the support provided.
Understanding the patient's emotional state is foundational for offering personalised care. Acknowledge the recent diagnosis and elicit the patient's thoughts, concerns, and expectations through open-ended questions. Patients may express a mix of emotions, including confusion, relief, and/or anxiety. This understanding forms the basis for a tailored and empathetic discussion.
A comprehensive understanding of the patient's general health history and the timeline of any presenting symptoms is vital. Explore symptoms such as fatigue, thrush, and urinary infections to create a clearer picture that aids in contextualising the diabetes diagnosis.In instances where the patient does not exhibit any presenting symptoms, this aspect should also be taken into consideration for a well-rounded assessment.
Simplifying type 2 diabetes is crucial for patient comprehension. If not already explained by the doctor, discuss how the body's inability to regulate sugar leads to elevated blood sugar levels and subsequent complications. Encourage patients to summarise the key points to reinforce their understanding.
Delve into both short-term and long-term complications, connecting them to the patient's experiences. Relate symptoms, such as urinary infections, to the underlying elevated sugar levels. Address specific concerns raised by the patient, such as potential eye and foot complications.
As the consultation concludes, provide educational materials for the patient to review at their own pace, being mindful not to overwhelm them. Encourage questions and emphasise ongoing support, ensuring patients feel empowered and informed about managing their condition.
Maintain a proactive approach by checking in with the patient each time they come to fill a new prescription. During these check-ins, pharmacists should delve into discussions about medication adherence openly. Identifying any potential issues the patient might be facing, whether it's forgetfulness, concerns about side effects, or challenges in integrating medications into their daily routine, is crucial. If forgetfulness emerges as a significant hurdle, pharmacists can introduce the concept of dose administration aids such as pill boxes or blister packs. This proactive stance demonstrates a commitment to the patient's overall well-being.
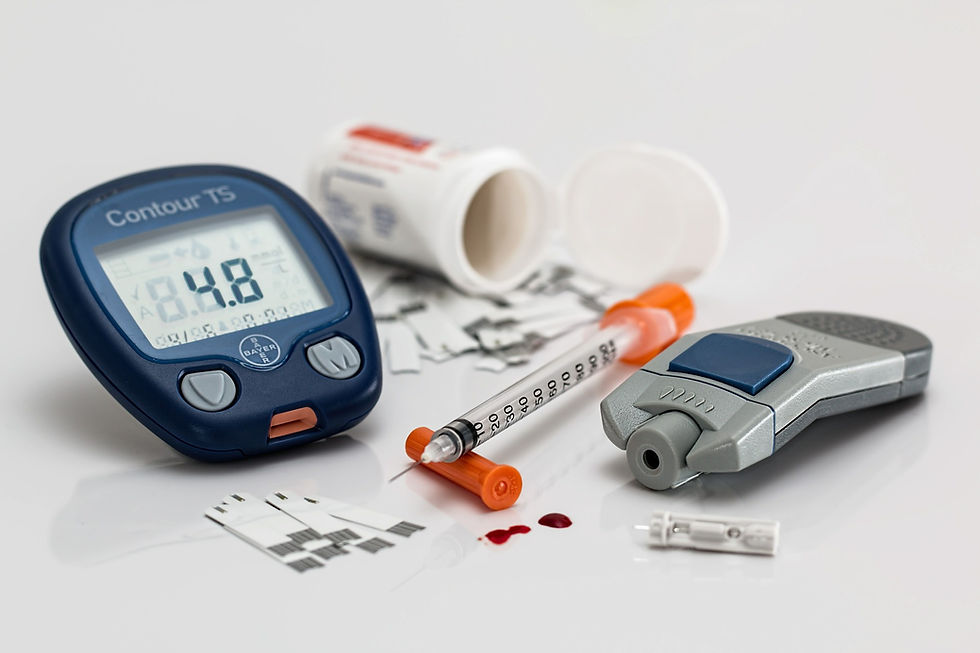
Understand the recommendations around blood glucose monitoring and inquire about the guidance provided by their doctor. Questions such as, "Will you need a blood glucose machine today?" and "How long are you required to self-monitor your blood glucose levels?" are instrumental in tailoring the support provided. If the patient is uncertain about the specific requirements or the operation of the device, this presents an opportunity for pharmacists to offer step-by-step guidance.
Should the patient express uncertainty or lack the necessary equipment, pharmacists can play a vital role in recommending suitable blood glucose monitoring devices. Provide detailed instructions on how to use the machine, including proper calibration, obtaining accurate readings, and the significance of understanding what the results mean.
Navigating a diabetes diagnosis transcends the transmission of medical information; it involves creating a collaborative and supportive healthcare environment. Acknowledge the patient's emotions, provide tailored education, and empower them to actively participate in their care.
Incorporating these strategies into diabetes consultations fosters a patient-centered approach, enhancing overall healthcare outcomes. Pharmacists, equipped with empathy and knowledge, become integral partners in a patient's journey towards managing diabetes effectively.
Key Takeaways for Pharmacists:
Establish Rapport: A compassionate introduction sets the tone for an effective consultation.
Explore Patient's Perspective: Understand the patient's thoughts, concerns, and expectations to tailor your approach.
Thorough History-Taking: Uncover the patient's medical history and any presenting symptoms for a comprehensive understanding.
Simplify Complex Concepts: Break down the pathophysiology of diabetes into digestible information, ensuring patient comprehension.
Relate to Complications: Connect potential complications to the patient's experiences, fostering a personalised and relatable discussion.
Provide Educational Resources: Empower patients with informational materials for continued learning and reference.
Maintain a proactive approach: Create an open channel for communication, ensuring patients feel supported and informed throughout their healthcare journey.
Discuss blood glucose monitoring: Explain the guidelines around blood glucose monitoring at home. If required suggest appropriate blood glucose monitoring devices that align with the patient's needs and preferences.

Comments